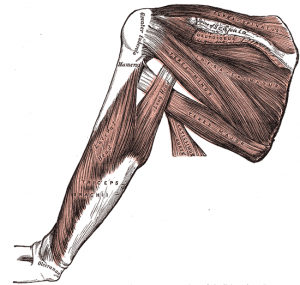
El manguito de los rotadores es un grupo de músculos y tendones que van pegados a los huesos de la articulación del hombro, permitiendo que éste se mueva y manteniéndolo estable.
- La tendinitis del manguito de los rotadores se refiere a la irritación de estos tendones e inflamación de la bursa (una capa normalmente lisa) que recubre dichos tendones.
- Un desgarro en el manguito de los rotadores ocurre cuando se rompe uno de los tendones a raíz de una sobrecarga o lesión.
Causas
La articulación del hombro es un tipo de enartrosis donde la parte superior del hueso del brazo (húmero) forma una articulación con el omóplato (escápula). El manguito de los rotadores sostiene la cabeza del húmero en la escápula y controla el movimiento de la articulación del hombro.
Los tendones del manguito de los rotadores pasan por debajo de un área ósea en su camino hasta fijarse a la parte superior del hueso del brazo. Cuando estos tendones se inflaman, pueden resultar más desgastados sobre esta área durante los movimientos del hombro. Algunas veces, un espolón óseo puede estrechar el espacio aún más.
Este problema se denomina tendinitis del manguito de los rotadores o síndrome de pinzamiento y puede deberse al hecho de:
- Mantener el brazo en la misma posición durante períodos de tiempo largos, como realizar trabajo de computadora o arreglo de cabello.
- Dormir sobre el mismo brazo cada noche.
- Practicar deportes que requieren movimiento repetitivo del brazo por encima de la cabeza como el tenis, el béisbol (particularmente el lanzamiento), la natación y el levantamiento de pesas por encima de la cabeza.
- Trabajar con el brazo por encima de la cabeza durante muchas horas o días (como los pintores y los carpinteros).
- Deficiente control o coordinación de los músculos del hombro y el omóplato.
La mala postura durante muchos años y el desgaste normal de los tendones que ocurre con la edad también pueden llevar a que se presente tendinitis del manguito de los rotadores.
Los desgarros del manguito de los rotadores pueden ocurrir de dos maneras:
- Un desgarro repentino o agudo puede suceder cuando usted se cae sobre su brazo mientras éste está estirado o después de un movimiento súbito o repentino al tratar de alzar algo pesado.
- Un desgarro crónico del tendón del manguito de los rotadores ocurre lentamente con el tiempo. Es más probable en aquellas personas con tendinitis crónica o síndrome de pinzamiento. En algún momento, el tendón se desgasta y se rompe.
Hay dos tipos de desgarros del manguito de los rotadores:
- Un desagarro parcial es cuando la ruptura no corta completamente las conexiones al hueso.
- Un desgarro completo o total se refiere a una ruptura del todo. Puede ser tan pequeña como una punta de alfiler o de todo el tendón del músculo. Los desgarros completos tienen desprendimiento del tendón desde el sitio de adherencia y no sanarían muy bien.
Síntomas
TENDINITIS O SÍNDROME DE PINZAMIENTO
Al comienzo, el dolor ocurre con actividades que se realizan por encima de la cabeza y al alzar el brazo hacia el lado. Las actividades abarcan cepillarse el cabello, alcanzar objetos en los estantes o practicar un deporte con movimientos por encima de la cabeza.
- El dolor es más probable en la parte frontal del hombro y se puede irradiar hacia el lado del brazo. Sin embargo, este dolor siempre se detiene antes del codo. Si el dolor va más allá del brazo hasta el codo y la mano, esto puede indicar que hay pinzamiento de un nervio.
- También puede haber dolor al bajar el hombro desde una posición elevada.
Al principio, este dolor puede ser leve y ocurrir sólo con ciertos movimientos del brazo. Con el tiempo, el dolor puede presentarse en reposo o por la noche, sobre todo al acostarse sobre el hombro afectado.
Usted puede tener debilidad y pérdida de movimiento al elevar el brazo sobre su cabeza. El hombro puede sentirse rígido al alzar algo o con movimiento. Puede volverse más difícil colocar el brazo por detrás de la espalda.
DESGARROS DEL MANGUITO DE LOS ROTADORES
El dolor con un desgarro repentino después de una caída o lesión generalmente es intenso. Con frecuencia, se presenta debilidad del hombro y del brazo junto con una sensación instantánea de movimiento.
Los síntomas de un desgarro crónico del manguito de los rotadores abarcan un empeoramiento gradual del dolor, la debilidad y la rigidez o pérdida del movimiento. El momento exacto cuando comienza un desgarro del manguito de los rotadores en alguien con tendinitis crónica del hombro puede o no notarse.
La mayoría de las personas con desgarros del tendón del manguito de los rotadores presentan dolor por la noche. El dolor que es peor por la noche puede despertarlo a uno. Durante el día, el dolor es más tolerable y duele con ciertos movimientos.
Con el tiempo, los síntomas se vuelven mucho peores y no se alivian con medicamentos, reposo o ejercicio.
Pruebas y exámenes
Un examen físico puede revelar sensibilidad por encima del hombro y se puede presentar dolor cuando el hombro se eleva sobre la cabeza. Generalmente, hay debilidad del hombro cuando se coloca en ciertas posiciones.
Las radiografías pueden mostrar un espolón óseo y se puede hacer en el consultorio médico.
Si el médico piensa que usted puede tener un desgarro del manguito de los rotadores, le pueden hacer uno o más de los siguientes exámenes:
- Una ecografía usa ondas sonoras para crear una imagen de la articulación del hombro. Con frecuencia, puede mostrar un desgarro en el manguito de los rotadores.
- La resonancia magnética del hombro puede mostrar hinchazón o un desgarro en el manguito de los rotadores.
Algunas veces, se necesita un examen imagenológico especial llamado artrografía para diagnosticar un desgarro en dicho manguito. El médico inyectará un material de contraste en la articulación del hombro. Luego, se usa ya sea una radiografía, una tomografía computarizada o una resonancia magnética para tomarle una imagen. El material de contraste generalmente se emplea cuando el médico sospecha de un pequeño desgarro en el manguito de los rotadores.
Tratamiento
TENDINITIS O SÍNDROME DE PINZAMIENTO
El tratamiento implica descanso del hombro y evitar actividades que causen dolor. Puede consistir en:
- Compresas de hielo aplicadas en el hombro 20 minutos a la vez, de 3 a 4 veces por día.
- Tomar fármacos como ibuprofeno y naproxeno para ayudar a reducir la hinchazón y el dolor.
- Evitar o reducir actividades que causen o empeoren sus síntomas.
Usted debe empezar fisioterapia con el fin de aprender ejercicios para estirar y fortalecer los músculos del manguito de los rotadores.
Si el dolor persiste o si la terapia no es posible debido al intenso dolor, una inyección de esteroides puede reducir el dolor y la hinchazón en los tendones lesionados, para permitir la eficacia de dicha terapia.
Con reposo y ejercicio, los síntomas con frecuencia mejoran o desaparecen; sin embargo, esto puede tardar semanas o meses.
La
cirugía artroscópica puede eliminar el tejido inflamado y parte del hueso que está sobre el manguito de los rotadores. Extraer el hueso puede aliviar la presión sobre los tendones.
DESGARROS EN EL MANGUITO DE LOS ROTADORES
Alguien con un desgarro parcial del manguito de los rotadores que normalmente no tiene mucha exigencia sobre el hombro puede probar con reposo y ejercicio.
Si el manguito de los rotadores ha tenido un desgarro completo o si los síntomas persisten a pesar del tratamiento farmacológico, se puede necesitar
cirugía para reparar el tendón. La mayoría de las veces, se puede usar la cirugía artroscópica. Algunos desgarros grandes requieren una cirugía abierta para reparar el tendón roto.
Pronóstico
Muchas personas recuperan completamente la función después de una combinación de medicamentos, fisioterapia e inyecciones de esteroides posterior a un episodio de tendinitis del manguito de los rotadores. Algunos pacientes tal vez necesiten cambiar o reducir la cantidad de tiempo que emplean con ciertos deportes para permanecer sin dolor.
Las personas con desgarros del manguito de los rotadores tienden a evolucionar bien, aunque el desenlace clínico depende altamente del tamaño del desgarro y el tiempo durante el cual éste ha estado presente, así como de la edad y del nivel de funcionamiento previo a la lesión.
Cuándo contactar a un profesional médico
Solicite una cita con el médico si se presenta dolor persistente en el brazo. Igualmente consulte si los síntomas no mejoran con el tratamiento.
Prevención
Evite los movimientos repetitivos por encima de la cabeza. Desarrolle la fuerza del hombro en grupos musculares opuestos.
Nombres alternativos
Hombro de nadador; Hombro de lanzador; Síndrome de pinzamiento del hombro; Hombro de tenista; Tendinitis del manguito de los rotadores; Síndrome de sobrecarga del hombro
Referencias
Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part II. Treatment. Am Fam Physician. 2008;77(4):493-497.
Burbank KM, Stevenson JH, Czarnecki GR, Dorfman J. Chronic shoulder pain: part I. Evaluation and diagnosis.Am Fam Physician. 2008;77(4):453-460.
Greiwe RM, Ahmad CS. Management of the throwing shoulder: cuff, labrum and internal impingement. Orthop Clin North Am. 2010 Jul;41(3):309-23.
Matsen III FA, Fehringer EV, Lippitt SB, Wirth MA, Rockwood Jr. CA. Rotator cuff. In: Rockwood CA Jr, Matsen FA III, Wirth MA, Lippitt SB, eds. The Shoulder. 4th ed. Philadelphia, Pa: Saunders Elsevier; 2009:chap 17.
Seida JC, LeBlanc C, Schouten JR, Mousavi SS, Hartling L, Vandermeer B, Tjosvold L, Sheps DM. Systematic review: nonoperative and operative treatments for rotator cuff tears. Ann Intern Med. 2010 Aug 17;153(4):246-55.
Actualizado: 7/6/2011
Versión en inglés revisada por: C. Benjamin Ma, MD, Assistant Professor, Chief, Sports Medicine and Shoulder Service, UCSF Department of Orthopaedic Surgery. Also reviewed by David Zieve, MD, MHA, Medical Director, A.D.A.M. Health Solutions, Ebix, Inc.
Traducción y localización realizada por: DrTango, Inc.